When I am asked about my future plans, my response is rightfully met with confusion. I am entering the workforce as an academic internal medicine physician devoting my practice entirely to the outpatient setting. Yet, two-thirds of my residency training has been managing patients within the walls of a hospital. That disconnect raises interesting questions about my career choice, and, naturally, makes me an anomaly among my peers.
According to the American College of Physicians Internal Medicine In-Training Exam, the number of residents planning careers in general internal medicine decreased from 54% in 1998 to 23% in 2007, with continued decline to 19% in 2015. Match those numbers with the fact that 60% of procedures and most patient visits occur in the outpatient setting, as stated by a 2014 Council of Graduate Medical Education report. In addition, many diseases are managed differently between the outpatient and inpatient setting, while some conditions, such as asthma and HIV, are not frequently treated in hospitalized adult patients. These incongruences certainly create concern.
Despite my usual arguments that ambulatory medicine offers the satisfaction of developing long-term patient-physician relationships, the pursuit of the diagnosis of complex illnesses, and focus on preventive care, a lack of resident exposure to a solid outpatient training will consistently trump efforts to focus on its appealing features. Thankfully, I had the opportunity to see its attractiveness, but only when certain environmental factors were in place during my training. I wish to shed some light on these elements with the hope that someday we can create more anomalies who meet the needs of our outpatient population.
The first element may seem obvious, but it is often missed in most residency training programs. In order to make outpatient medicine attractive to residents, there needs to be a focus on education in that setting. To elaborate, the clinic needs to be treated with near equal importance as the wards in terms of devoted patient care efforts and strength of curriculum. I will not argue for an equal split of time spent between the outpatient and inpatient realms primarily due to the issue of team coverage and the required time it takes to develop the ability to identify critically ill patients. However, protected time should exist to focus on patient care while in the clinic.
Throughout my residency training, I worked within the 4+1 framework where I had a scheduled week of clinic every four weeks that was devoid of inpatient responsibilities, including pager call or rounding on patients in the morning. This schedule allowed me to focus on clinic concerns without hospital patient care overshadowing my thoughts. An ideal learning environment was created with space to refine my skills in managing outpatient conditions.
In addition to devoted time in the clinic, an importance placed on ambulatory curriculum improves the educational environment. This includes academic time dedicated to teaching the proper management of chronic illnesses and the intricacies of ambulatory health systems. In addition, resources to aid career development for those interested in ambulatory medicine should be an important component of the curriculum. During my clinic week, I would participate with other residents in clinic-specific noon conferences that operated independently of the inpatient conference. The curriculum covered the management of common outpatient conditions with the use of the Yale Office-Based Curriculum modules, the critical analysis of journal articles concerning chronic illnesses, and the proficiency of office-based procedures with utilization of simulations including point-of-care ultrasound. With the emphasis the program placed on promoting an ideal educational environment in the clinic, I saw ambulatory medicine as possible career choice and was comfortable managing patients in this setting.
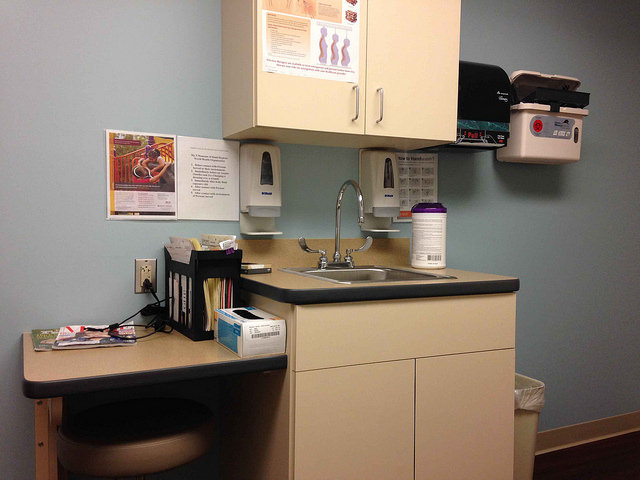
In addition to having a strong academic focus, the clinic needs to be well-run from an organizational standpoint. Resident clinics are notoriously disorganized, slow and inefficient. During training, residents need exposure to a clinic system that incorporates the multiple disciplines required for a well-functioning environment. While my program’s clinic had inefficiencies, I also saw continued improvement in its operations throughout my residency. Team-based care became an important feature as nursing staff, patient service representatives, social workers and care managers played a role in communicating with patients, completing prior authorizations and durable medical equipment certifications, and ensuring patients had appropriate preventive care. Also, continuity of care between physicians and patients was emphasized with special attention given to consistent appointment scheduling. Stable working relationships between nursing staff and doctors were also stressed as each nurse and resident was assigned to one another. As a result, resident and nurse preferences were understood which led to more effective patient care and greater staff satisfaction.
Even experiences outside a resident clinic, including faculty private clinics, grant insight into the variety of ways to practice outpatient medicine. My program dedicated one half-day during each resident’s clinic week for him or her to work in the private clinic of a faculty member. When I co-managed patients with my designated attending, I learned techniques to improve my efficiency and clinical decision making. Additionally, I gained an example of job fulfillment in the ambulatory setting, which was one of the most important influences on me when I was considering my vocation. The classic resident lamentation of a poorly-designed clinic structure can be minimized by showcasing an efficient, effective and satisfying system. If this is done well, there may be more anomalies yet.
Finally, one of the necessities to recruit residents into outpatient practice is a competitive salary and work-life balance. The recommendations made up to this point are valuable during training. However, unless compensation is adequate, it will be difficult for trainees to throw clinic medicine into the ring of career options.
In a 2019 Merritt Hawkins Inpatient/Outpatient Revenue Survey, the specialties of internal and family medicine, which contain the bulk of ambulatory practitioners, have the lowest percentage of salary compared to generated revenue. Rather than an indictment against physicians, the role of finances in doctors’ occupation choices serves a good reminder of where the health care system places its value. This is especially true when concern over student loan burden and work-life balance are typically at the forefront of resident minds.
In order to quell any misunderstanding, I acknowledge there should be some disparity of incomes among health care professionals given work schedules and length and difficulty of training. However, the current system typically disincentives the positions where the majority of our workforce is needed. I do not mean to launch into a diatribe over the undervaluing of outpatient primary care physicians in our system. I do have hope insurance reimbursement and, consequentially, salaries for front-line doctors will continue to improve with value-based payment reform. In the meantime, residency programs can steer their housestaff to loan repayment programs available to those interested in outpatient medicine and primary care. Many times these programs open career opportunities to physicians who would find them impractical due to financial concerns. Luckily, the compensation for my chosen job is fairly competitive with some of my colleagues pursuing inpatient positions, although there still remains a pay cut. However, I trade a higher salary for weekends and holidays off, as well as schedule flexibility to pursue my academic interests. Although an ambulatory primary care physician may never have the same financial compensation as a neurosurgeon or possibly even a general hospitalist, residency programs, hospital systems and private practices need to ensure those interested in outpatient medicine are not barred due to concern over inability to afford their desired career path.
Deliberate efforts are required to ensure training in outpatient settings does not come as an afterthought to hospital rounds. My experience with strong ambulatory curriculum, an outpatient environment conducive to learning, well-run clinics and scheduling and financial compensation that aligns with career goals drove me to a path many of my internal medicine colleagues tend not to choose. While being an anomaly might seem special, I hope more can see the rewarding nature of a career dedicated to serving the majority of patients where they are — in the clinic.
Image credit: St. Mary’s Hospital Thyroid Exam Room by Steven Depolo licensed under CC BY 2.0.