Do you view residents in other departments as your extended family? Do you view your co-residents as your social support system?
Calling your grandma or inviting your estranged uncle over for Thanksgiving may not always be your natural inclination, but you do it because they are family. You learn to tolerate and even to accept their annoying eccentricities as lovable quirks.
Similarly, calling a surgical team for a consult does not have to be scary, and understanding that your emergency medicine colleagues go about decision-making differently can reduce frustration. Instead of jumping to stereotypes and judgments, you can reframe these interactions if you put them into context.
Early in intern year, I reached out to residents in other departments who were part of my patients’ care in the hospital. In an effort to redirect my thought patterns, I asked them how and what drives their interaction styles and their medical decisions.
An emergency medicine resident explained antibiotic choice based on risk-stratification by acuity, with broader coverage for sicker patients. An emergency faculty member highlighted that decisions are made with the available information at the time and that tests are sometimes ordered for the anticipated needs of the admitting team. These decisions are fueled by an overly burdened emergency department with long wait times for patients. Admission delays occupy beds and prevent treatment of the next patient.
A surgical resident described his call schedule while on the consult service: 24-hour call every four to five nights for 12 to 18 straight months. Overnight, he is the only surgeon in his field in the entire hospital, and he is also in charge of all consults for the hospital and the emergency department. While he would love to communicate with each team through conversation, he explained that his time constraints prevent this ideal, and he has to resort to whether or not the patient requires surgery.
Emergency medicine and surgery residents think and approach patient care differently than internal medicine and pediatric residents. Consults services are the lightest rotations for me, with weekends off and certainly no pages overnight. Our focus is on making careful treatment decisions and on coordinating discharge with interprofessional teams, but we are assessed on preventing rehospitalization rather than reducing emergency department wait times.
We all started in medical school, yet we quickly claim the identity of the field of our residency. We quickly assimilate to the stereotypes that pervade the hospital. These silos are omnipresent in academic medicine. Yet they fail to consider that these are artificial separations of the same crop. We all graduate from medical school with the same basic competencies, yet are harvested into surgery, family medicine, pediatrics, anesthesiology. Somehow, we quickly forget the same wheat from our alma mater and, in doing so, lose the ability, desire, confidence, or time to communicate with our colleagues in other departments.
All physicians welcome the chance to be understood, to be heard. Before jumping to assumptions, remember that your colleagues value patient care and have reasons for their medical decisions. Rather than dismissing them immediately, invite them to the table.
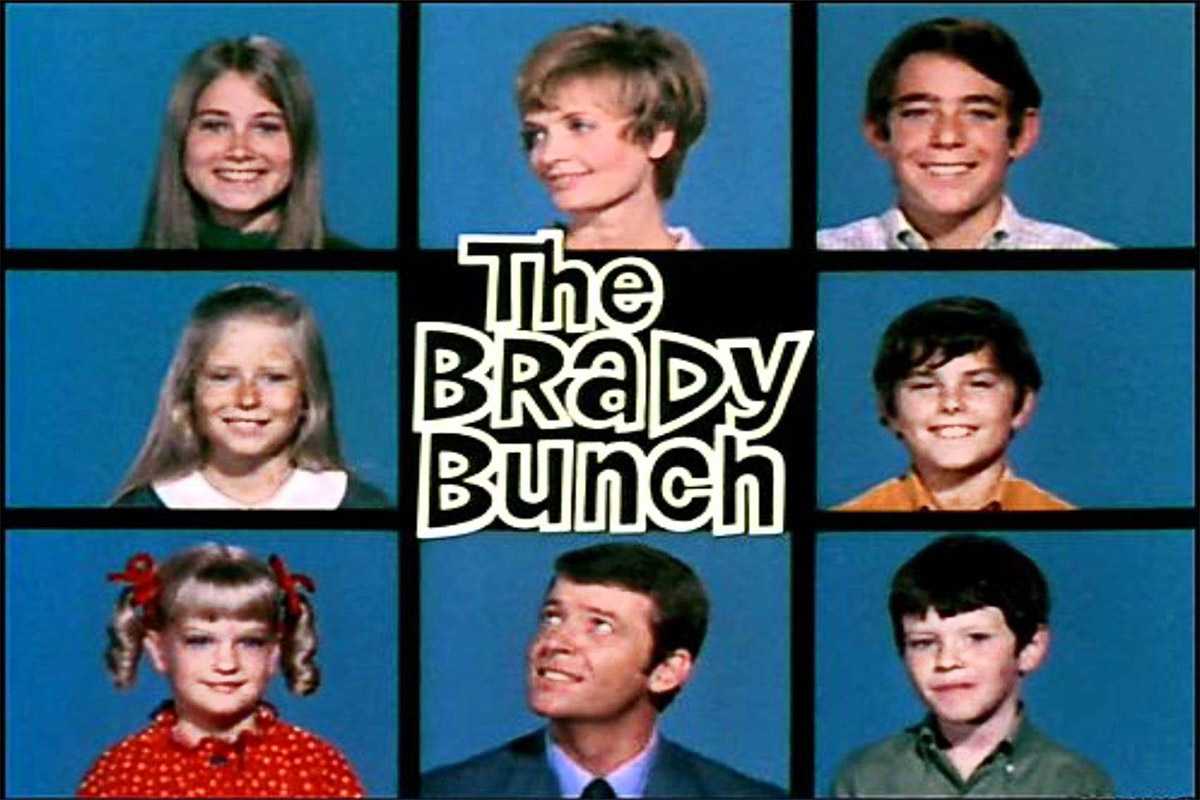
In light of recent press on resident burnout and depression, The Med-Peds Bunch explores the lived social support systems of a current Duke resident. Come join Austin as he begins his med-peds journey and reflects on feelings of family in residency.