by Dr. Katie Rief, MD, physical medicine & rehabilitation resident physician in New York City, written for COVID-19: Inside the Global Epicenter: Personal Accounts from NYC Frontline Healthcare Providers by Krutika Parasar Raulkar, MD
Day 50 something? I haven’t been counting. I had to look it up, from the first day we got the hint things were really wrong … March 3, 68 days ago. That was the day all domestic travel to conferences was banned.
By the next week, our first ever chief resident meeting, March 10, was the first and last time I’ve been in the same room with our leadership team. Following March 10th, we made the decision to suspend in-person didactics. HSS (Hospital for Special Surgery, one of our program’s affiliates) shifted to all remote learning as well. And then on March 18, HSS suspended all outpatient clinics and elective surgeries.
Programs scrambled to redeploy doctors and nurses, reorganize staff and expand ICU capacity. The hospital system expanded ICU bed capacity from 422 to 970 in 19 days. Incredible.
I worked my first shift in the emergency department on March 27 and continued there until mid-May.
Life in New York City shut down, but thank God, I could still go to work.
Personal protective equipment was scarce throughout, but in mid and late March, at critically low levels. Fear combined with poor health literacy meant much of our supply was wasted on people not in direct patient care roles. I wore the same N95 mask for a few shifts at a time. Nothing compared to hospitals where they wore them for a week or more. Products designed to be single use, one encounter. Compared to places like Elmhurst or Queens, we were in great shape. Columbia was hardest hit in mid to late March. As overwhelming as it was in some ways, it was also algorithmic.
What’s the oxygen sat? If less than 90%, add nasal cannula (NC), no more than six liters because it could create more aerosolization. If still less than 90%, add a nonrebreather (NRB). Once you are maxed out on six liters of NC and 10 liters of NRB, call the ICU — the patient will likely be intubated at some point. Utilize awake proning, essentially rolling people around until they tire out and need a definitive airway.
So much to process. I am thankful beyond belief — to be in it, to be helping, to be working, to be learning. I get to be in the ER, forever my favorite place in the hospital.
It is unnatural being stuck inside for so long. Disconnected from community. No circus, no gyms, no bars or restaurants. No happy hour, no sports. It rained all of April. Truly the cruelest month. Mental health has suffered dramatically — I care for so many more suicide attempts on shifts these days. Our own Dr. Lorna Breen, site director for the Allen Hospital, took her own life last week.
I miss my family. I miss the people I love. Maybe I should be more concerned about getting the virus, but I’m not. In all likelihood, I would be miserable for a week and then recover.
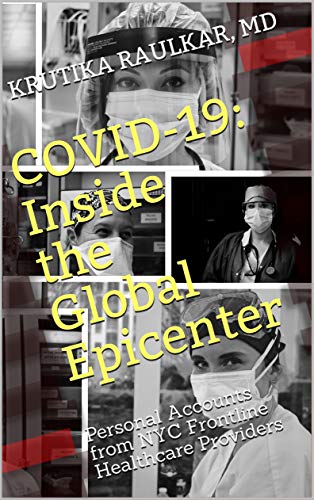 In her book COVID-19: Inside the Global Epicenter: Personal Accounts from NYC Frontline Healthcare Providers, Dr. Raulkar shares insider accounts of the deadly pandemic from one of the hardest hit medical systems in the world. Packed with the most current medical information, a historical account of the discovery and political reaction to COVID-19, and inspiring accounts and photos of frontline health care workers, this book provides the knowledge you need to stay well-informed about COVID-19, and hope and optimism to get you through these challenging times.
In her book COVID-19: Inside the Global Epicenter: Personal Accounts from NYC Frontline Healthcare Providers, Dr. Raulkar shares insider accounts of the deadly pandemic from one of the hardest hit medical systems in the world. Packed with the most current medical information, a historical account of the discovery and political reaction to COVID-19, and inspiring accounts and photos of frontline health care workers, this book provides the knowledge you need to stay well-informed about COVID-19, and hope and optimism to get you through these challenging times.


