When I first met Rita, she didn’t make things easy. She fired a barrage of questions at me, punctuating her litany with the dreaded blow to every resident’s ego — “Are you a student?” — before slouching back on her bed, sweat glistening on her gray-streaked temples as though she had run a marathon.
Feeling a combination of irritation and anxiety, as I had many more patients to see that morning, I failed to grasp how helpless Rita must have felt, lying amidst the chaos of IVs and monitors in a step-down unit. Two months ago, she was diagnosed with metastatic gastric cancer, and today I would tell her that she had suffered a stroke. This formerly independent elderly woman, who lived in her own apartment, cooked for herself, and attended all of her appointments on her own, was grasping at what little control she had in the face of sudden debilitation. Unfortunately, all I saw in front of me that stressful morning was a stubborn old woman who refused to accept the role that her illness was forcing upon her.
Though Rita’s neurological deficits resolved, her organ systems began to fail one by one. As a relatively new intern, I felt trapped beneath the weight of my role as Rita’s physician. I was meant to restore her back to self-sufficiency, yet new problems kept arising against the ominous specter of her cancer.
The sense of powerlessness that consumed me brought me back to another hospital room almost five years earlier, where my father lay, also in the clutches of advanced cancer. Suddenly, I wished I could sit next to Rita for more than five minutes and listen to her as she shared her hopes and desires. Perhaps a part of me wanted to resurrect the words that were left unspoken as I watched my father succumb, losing every semblance of humanity. Yet at the end of the day, I had a job to do, and my days were ruled by the rush of pre-rounding, answering pages and putting in orders. There was little time to ask Rita about more than her ability to sleep, eat, breathe or go to the bathroom.
Unfortunately, Rita’s words began to make less sense with every passing day. The palliative care team visited her, and after a long discussion, she agreed to not be resuscitated in the event of cardiac arrest, given the advanced stage of her cancer. Perched on the precipice of death, but with no viable ways to keep her alive, Rita was all set to be discharged home with hospice care.
I visited Rita the next morning and noticed that something was not quite right. Instead of telling me she was in the hospital, she mumbled something about being at home.
I stopped cold as the image of my father crept into my consciousness again. He was propped up in his hospital bed, barely able to string words together as he refused a breakfast tray. Just days before, we had discussed how to finance medical school.
I hurtled back to the present upon hearing Rita’s voice again. “My daughter’s friend … coming. Don’t … like … him.” With what little strength she could muster, she shot me a conspiratorial smile. I left her room, shaking, and immediately called my attending. We drew a STAT ammonia level and confirmed the cause of her cognitive deterioration. My attending then called Rita’s daughter to convey the damning news.
I knew, from my experience with my father, what Rita would look like with each step closer to death’s door. After the confusion came the silence. Eyes closed, mouth ajar. Breathing steadily, appearing almost to snore. My father had, at one point, squeezed my hand and my mother’s, as if to challenge the gatekeepers of the afterlife. I saw Rita similarly reach for her daughter with one hand. Moments later, her other hand twitched in what seemed like a dismissive wave at her daughter’s boyfriend, who was standing on the other side of the bed. Even in the twilight of her life, she remained a concerned, protective parent.
Just before I entered Rita’s room on her final morning, I heard her daughter’s tearful voice rise above the whirr of activity in the hallway. “I’m so sorry, mommy, for not always being there.” She took a ragged breath, composing herself before uttering another apology as I entered the room. Seeing her leaning forward towards her mother with hands clasped in prayer, I could not help but shed all professional appearances. I laid my arm across her shoulders. “She loves you,” I said, turning to look at Rita, who appeared to be suspended in a deep sleep, much like my father had just before he passed. “No matter what, I promise that she loves you.”
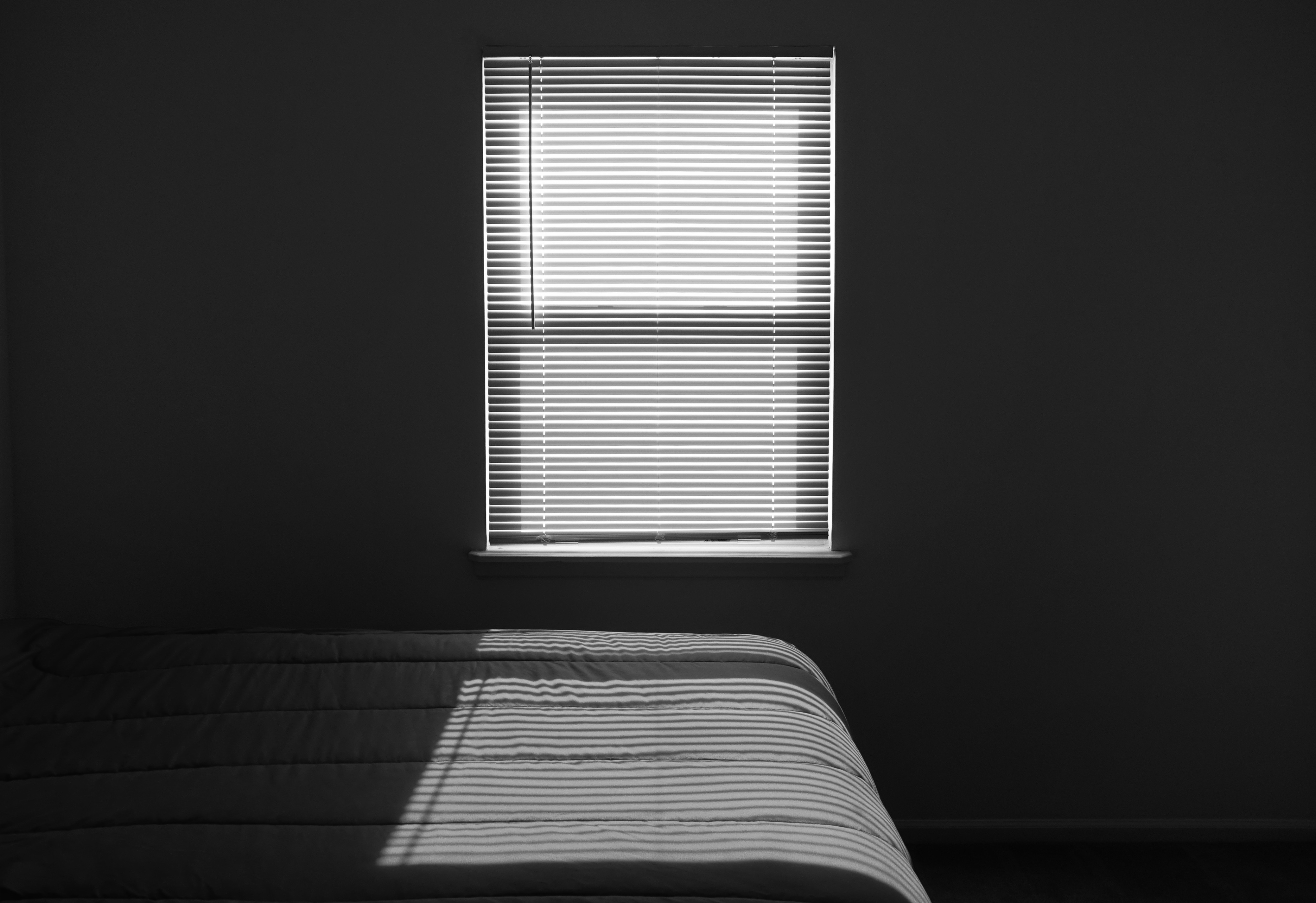
The next day, I passed by the room to see an empty bed, pristine white covers tucked neatly into the sides. All traces of death vanished, the bed awaited a new occupant, and I awaited a new addition to my census.
When faced with a revolving door of patients, it is easy for us as physicians to overlook each one’s losses. Rita briefly lost her voice to the stroke that landed her in the hospital. She lost sleep every time the nurses had to draw her blood and check her waning vitals. Most of all, she quickly lost her agency, as she went from taking care of her medical needs to having to communicate her needs to others, myself included, who could not always give her what she wanted. During the week that I cared for Rita in the hospital, I regretted the time constraints and anxieties that distracted me from listening to her more deeply and, perhaps, attending to her needs more calmly. That loss of meaningful time spent with Rita was something I glimpsed in her daughter, and something I recalled from my own experience with my father.
We may never be able to offer our full selves to our patients, given the bustling nature of our profession. Nonetheless, I hope that we can make every effort to be present with them and acknowledge all that they lose by taking on that dreaded role. I hope we can set aside the smothering pressure to perform and view our patients with compassion and empathy, even when their illnesses render us helpless, unable to restore their losses.
Author’s note: All names and identifying information have been changed to protect patient privacy.
Image credit: room by Dean Hochman is licensed under CC BY 2.0.