The following manuscript was submitted to the October 2018 Complications theme issue.
“If we can continue to wean him like he’s tolerating now, we should be able to extubate on Friday.”
The first thought that entered my head? Not the one you’d probably guess.
Shit.
By anyone’s standards, from a medical perspective, we did everything right. But all I could think about is how much we hurt this boy by saving his life. How we saved his life just enough, not to kill him, just to take away every meaningful part of human existence.
Maybe he could breathe on his own. Maybe his heart could continue beating. Because he was only eight years old, after all. His body was plastic. Resilient. And sure, his brainstem would continue functioning. That most basic part of our human brains, buried down under layers of cortical brain tissue and dura and skull and scalp and hair. As protected as God or evolution or both could make it. Hidden down there to keep it safe, keep it from harm. Keep our hearts beating. Keep the muscles of our chest wall contracting, allowing air to continue to enter our lungs, the blood pumped by our heart rushing by and carrying blood and oxygen to the rest of the body. He’d be alive, sure.
But what life?
Our patient’s brain had herniated one week earlier. His brain had swelled. The tissue expanded. Surrounded by rock solid skull, that swelling tissue eventually has nowhere to go. Pressure rises. Eventually, brain goes through the only space it has to go through, a small hole in the bottom of our skulls that connects our spinal cord to our brain, our brain to the rest of our bodies. Lava through a volcano.
In the process it applies pressure on every other vital structure that enters that space. Nerves, blood vessels. Blood vessels. Blood is no longer effectively flowing to our patient’s brain. He has a stroke. Not just any stroke, a massive stroke involving almost the entirety of his cortex. The English language, gone. Memories of his first day of school, gone. His smile. His ability to enjoy that first sip of freezing cold water after running around the soccer field on the first warm spring day, gone. Speaking. Eating. Thinking. Laughing. Loving. All gone. Breathing, beating. Remain.
How do we, his physicians, respond? How do we fix it? Our patient has a bitemporal craniotomy. We remove two big chunks of his skull on each side of his head. We do what we as a medical team are expected to do, we perform lifesaving measures for our patient. Brain now has space to expand out instead of down. The brainstem is saved. Breathing. Beating. Remain.
Our lives as we know them are not just the beating of our hearts and breathing of our lungs. Our lives are waking up every morning and seeing the sunrise. Our lives are a hug from our mother after a long and tiring day. A nap on the couch with our dogs. A run through Central Park, breeze blowing through our hair. The first ice cream cone of summer. Our lives are the interlacing of experience and human interaction that weave a beautiful web. These are the lives we as physicians strive to save every single day. To get a child to their first day of kindergarten. To get a grandmother to the wedding of her first grandchild. We strive to enable more life, more love, more joy.
But in this age of medicine, where technology and knowledge have so advanced, what happens when we miss our mark? What happens when we keep a heart beating and lungs breathing, but life is gone? Is breathing and beating enough?
Recently, I was at a medical museum, in a room explaining the discovery of x-rays and their early use. I remember looking at a poster board, reading about how doctors initially used x-rays in attempts to treat many ailments. They irradiated skin in an attempt to cure various skin lesions, only to worsen them. Women even used x-rays as a method of facial hair removal until they started developing head and neck cancers. I remember marveling to myself, how amazing it was what we didn’t know. How we dangerously harnessed this new knowledge, how we caused harm in an attempt to do good. And then I thought to myself, with what practice are we doing this today? Where are we overshooting?
As we jump into the beginning of our careers, as residents, it is easy to want to do it all. I am a pediatrics resident, and in my field it is more prevalent than ever, so understandably so. I more than understand the drive to stop at nothing to save a life. I have that drive. Cure all. Save all. Fix all. We enter medicine not just with the desire to heal, but to heal always. But as we advance in our careers and we begin to develop our own styles of practice, it is important to remember what you are fighting for. We have at our fingertips the capability to do many incredible things. To keep neurons firing and lungs breathing and hearts beating and kidneys filtering. But take a step back. Know your patient. Know that person and know their family. Ask them what they want. What is life to them? What do they want us to save?
At the end of the day, what remains?
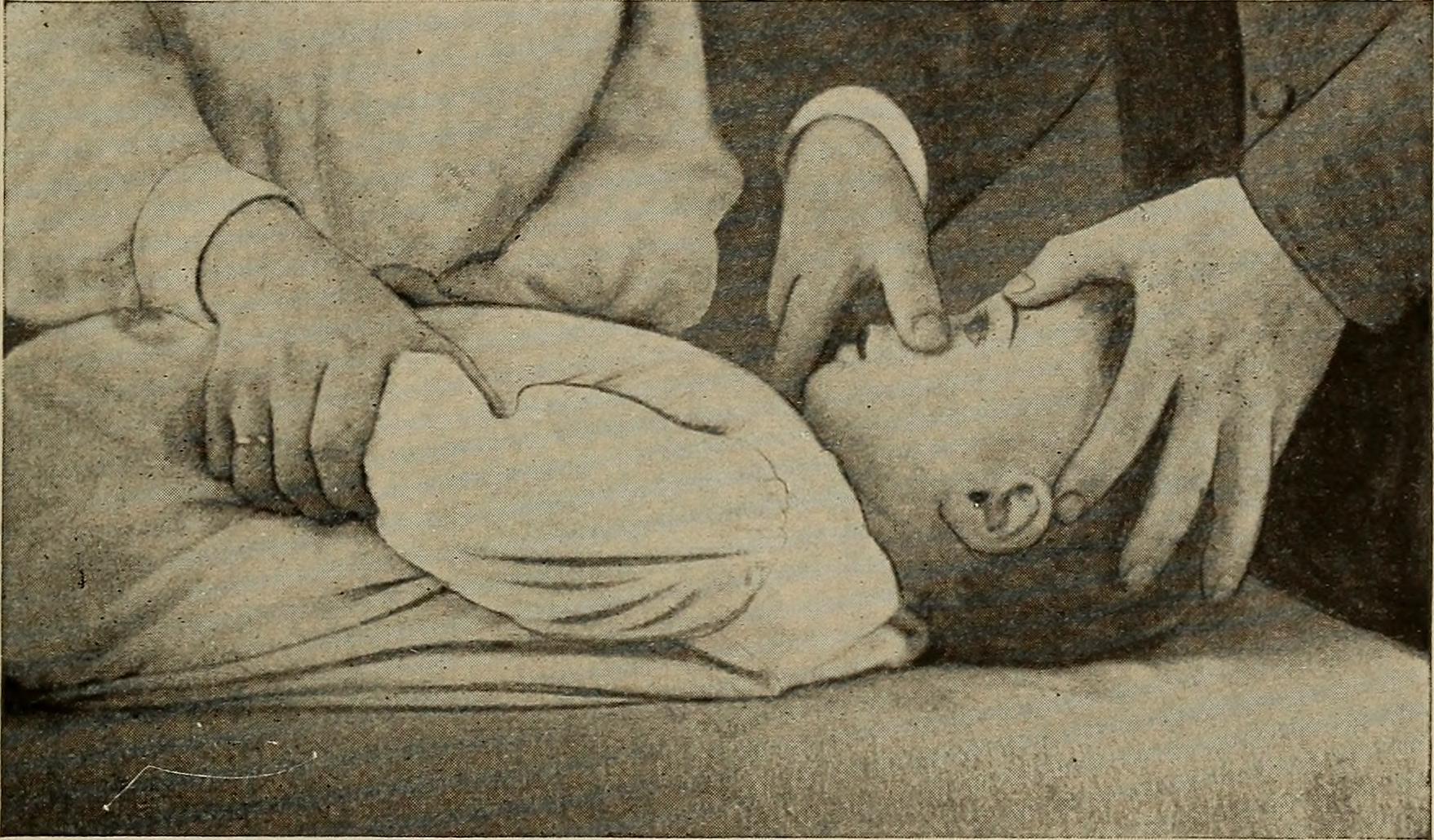
Image credit: from Diseases of Children (1916) licensed in the public domain.