The following manuscript was published as part of the March 2019 s/p The Match — One Year Later theme issue.
This week, tens of thousands of medical students match to a residency, much in the style of Colton Underwood concluding his Bachelor journey. Rejected by his first-choice love in the Fantasy Suites last week, Colton ran away from the producers in shame, which segued strangely nicely into the season finale of The Good Doctor, where an anguished Dr. Shaun Murphy spoke his truth to doctors who transferred him from his beloved surgery to my clinical specialty, pathology, citing poor people skills.
“I don’t want to be a pathologist!” he yelled.
I didn’t, either. As on the show, per Murphy’s Law, a boss passed on my name.
On St. Patrick’s Day 2014, New York’s coldest in a decade, I was a grass snake banished from the fair isle of pediatrics. In the National Residency Matching Program, just half of one percent of approximately 2,500 pediatrics slots across 194 programs remained unmatched, something like four total positions nationwide. It had been a full century since anyone in my family had practiced medicine, and I, despite longstanding interest in toxic chemical exposures in children, joined the club with my Irish, Bellevue-trained great-grandfather who drank himself out of practice. The world went from shrieks and spit-up to clot and poop, my thought through the cardiogenic prodrome a line from my old boss:
“You went to Yale,” she said of my shambolic fifth-grade science classroom. “You’ve never failed at anything in your life!”
No one knew why the wind blew in my face. My scores and grades were fine. No one maligned my character. From 30 applications, 12 programs invited me to visit, which ended up costing hundreds of dollars in travel expenses. Interesting, interested interviewers offered water and tea for our worn mouths and free cocktails and friendly dinners for trainees. My true preference had the fewest positions. I ranked seven others I could live with, as instructed, but it worked out that I liked them all. I matched at none.
The Match’s Supplementary Offer and Acceptance Program (SOAP), or “Scramble,” leaves a week to secure unmatched openings. Voice shot, I faked strong, asked all day for three days straight if I’d ranked too few programs, auditioned at competitive ones, or applied in preventive medicine, earlier ruled out at the suggestion of my public health mentors, who said I liked inpatient time and it was important. Program directors in child neurology, psychiatry and internal medicine asked how I found their pile, then extended offers to other people. On Match Day, the school decked out a waterfront terrace with silk leis, balloons and champagne. Friends on research sabbaticals and old classmates immersed in intern year indignities stopped by or texted in. Advisors fanned out offer envelopes like card tricks. Dressed for career death in a coral sheath, I covered up, made brief hellos, then slunk home bawling, a woman magicians had cut in half. Heartbroken and ashamed, I would not set foot in a pediatrician’s office or inpatient ward for four years.
The first two months, I woke each morning to listless laundry heaps, world-hurt written on my face. Despondent, I bought off-brand scrubs online, then cut them off of my body. It was absurd, how sad I was to lose a job in an institution in which I and so many had lost faith and phoned in, preoccupied with identity crises. Our work, humiliation from threats and mistakes and overdosed titans, terminally-ill hipsters, aging incarcerated, celebrity stalkers, my failure to show up for others. Whether or not I was a good doctor, I identified as one, and not matching was self-fulfilling prophecy. Whoever pulled the shade in which I thought I had it made was God’s kick in the glutes for expressing my discomfort with the system and personal shame in polite company.
Never too busy to indulge my boring waffling, colleagues encouraged me to approach the Match as an unfortunate setback. I sought soul-crushing feedback and a root cause analysis. Information sharing was apparently against the rules, and as a potential re-applicant, I didn’t challenge that. From second-hand impressions, I was the common denominator, a diagnosis of exclusion. At the top of the differential were nerves and numbers. One doctor I knew as a premed said I “looked terrified” at my first interview. Another well-meaning doctor at home said others maybe minimized my quavers and mumbles, “to be nice?” A few observed the way I trailed off after rapidfire patter. They speculated that my nervous temperament might have struck certain listeners as incompatible with children. I never saw proof, but who knows. Some rang true, and they meant no harm. For me, though, that feedback that I lack some people skills persists like tinnitus.
There was nothing I could do to change my life or bulk my resume, they said, urging me to reapply after coaching, anxiolytics, and treatment for reflux laryngitis chronic cough. Reluctant to be anyone’s chore, I refused interventions and a postdoctoral research stint. Mentors called my bluff, somehow mobilizing contacts from all over the country in disparate specialties, some with no relationship or incentive. I had no plans and no excuse not to listen. They invested time in me as they would in a patient, telling me how to live for work when I had no desire to live, period. I wasn’t sure I had their vocation, but I felt I owed it to the next student or patient in my jam to try.
For weeks, I perused openings, some free, some subscription. No offers came, and I was ineligible for some public health jobs without a license, which requires one year of internship. By early May, I was begging. Miraculously, I caught wind of an unexpected July 1 opening at home in pathology, maybe the last one left. The specifics, which I don’t know, could involve a resident’s failed exam, background check, visa issue, or family emergency. Accepting felt unfair, but a program one intern short was unfair to patients. So, dumb luck. Why not practice the death I was living? I said yes during graduation week.
It was square one, the glass slide cover slip. I was trained in ergonomics, not microscopes, and had just come off a protracted odyssey to on-boarding paperwork. Between bureaucracies, dissection station steel clanged like a cafeteria, me on the phone forever in what a mortician said sounded to him like a senator. Caked in feces and blood, eyes rubbed raw with ragged nails, I was a pity invite to the misfit table. By some sick joke, my first four autopsies were neonates, their marbled skin swaddled, swollen, and stuffed with tubes. Three died of necrotizing enterocolitis, guts surgically adhered or distended with free air. Skin sloughed at first gloved touch. Our tool scratches sounded like Psycho orchestration, our probes bird beak picks. Caps cooled their brains, impressions that persisted when removed and prepped for transport through backrooms. Personal protective equipment soaked, we washed bile from workbenches with handheld nozzles, midway game targets sprayed in a crazed race to the bell.
Back in the lab, I learned the one true prerequisite to pathology practice, and it’s not managing machines. It’s empathy and people skills. Pathologists run large teams that fix more patients than most docs do. Some of them they even see. Training is a master’s in interpersonal relations, not just what The Good Doctor correctly described as detectives to beat cops. A better comparison might be editor to a writer, or psychoanalyst to patient analysand. The pathologist manages the style and cost of the diagnosis, communicates intelligible results, and soothes fellow practitioners’ ruffled feathers, talking surgeons like the ones who insulted Dr. Murphy off the ledge.
I don’t use that expression glibly, but as a graduate of a medical school at which three acquaintances died by suicide in the post-Match period. There is no way I can know their motivations. In the aftermath, I got a close view of what it’s like to keep working through devastation. Medical shows like The Good Doctor rarely portray that emotional havoc, endemic in this profession, and I was very touched to watch it.
Pathology, as it happens, celebrates difference, and is sensitive as a specialty to doctors mismatched with the world. Many among its ranks did not want to be there and ended up there by various structural flaws. Some were surgeons in other countries. Others missed bench research, or flexibility to raise their families. As lab license holders, we’re enervating and compulsive, but that’s because we contend with profound stress and disappointment while responsible for life-and-death decision points with small margins of error. I am reminded of a line in the great postwar Irish novel, Máirtín Ó Cadhain’s Cré na Cille, in which a county parish plot’s status-conscious corpses compare luck in past lives: “We here in the graveyard clay are the true democrats,” one says.
It was about impossible to reach that Zen that post-Match. Flustered, I stewed and second-guessed through shifts, wracked by ailments that sent me sprinting to bathrooms, then back out, paged with new mistakes. When someone called or didn’t, I’d evinced incompetence. The wellness-minded said pressure to impress was self-imposed, that no day passed without progress. I derived no satisfaction, sure only of my off-putting presence. No matter how many department supervisors sympathized, someone died every day, and I could not focus on them in the manner they deserved, still a skittish ingrate watching forensics experts give child abuse trial testimony unfazed. Self-flagellant, I found work a failed not guilty plea, and me selfish for the feeling. For showing up, I racked “developmental milestones” and was board-certified last June to copious tears.
Like a terminal illness or bankruptcy, failure to match crushes spirits. In some cases, it ends careers, that of the lowest ranking in the class, Harvard valedictorian, or an international graduate victim to a test in a second language or a capricious, racist Muslim ban. The Match, built to mitigate unfair advantage, is no longer a leveler. Applicants who can afford exorbitant fees get choice cush gigs. Those who can’t game the system don’t drip into underserved communities. Matches don’t guarantee happiness, either. The academic year transition exacerbates pervasive feelings of inadequacy, isolation and exhaustion, which people are ashamed to express as everyone puts game faces on for Match Week mania. Despite my gratitude for my savings, support, and connection, it angers me that not everyone has that. If they were guaranteed these, it would go far to make Match season much less miserable, and lessen the need to keep real characters like Shaun Murphy risking the hospital money by putting him out in public.
Pathologist is not an insult, but it’s not for everyone. I favor redistributive overhaul to maximize everyone’s means: eradicating student debt; full federal tuition; less biased background checks. Good faith efforts to complete training should be sufficient, disqualifying exclusions rarities. A free market is unlikely to distribute doctors where they’re needed. Programs are unprepared for candidate volume, advisors untrained in market vagaries, and unlike most trainees, I know that from experience. States accredit new schools and class sizes continue to grow, while residency slots fail to catch up. Many unmatched live ashamed and jobless for years despite no “red flags,” no documented ethical breaches, no underperformance. They just got unlucky.
Unmatched applicants will hear well-meaning doctors operate out of their impulse to heal. They’ll fix what they can, say that suffering is meaningful. What we must fix is a system of undue suffering, in which no one can afford choice or risk expressing shame and anger in full flower, worried even in tepid wellness initiatives that doing so is inappropriate or unprofessional. The Match has become paradigm for the physician as expendable commodity. Fixable structural failures create that treatment and Match season mood. It is a very Irish one, granted, but in that spirit, may the road to residency rise to meet all upon it. Your honesty might save a colleague’s life.
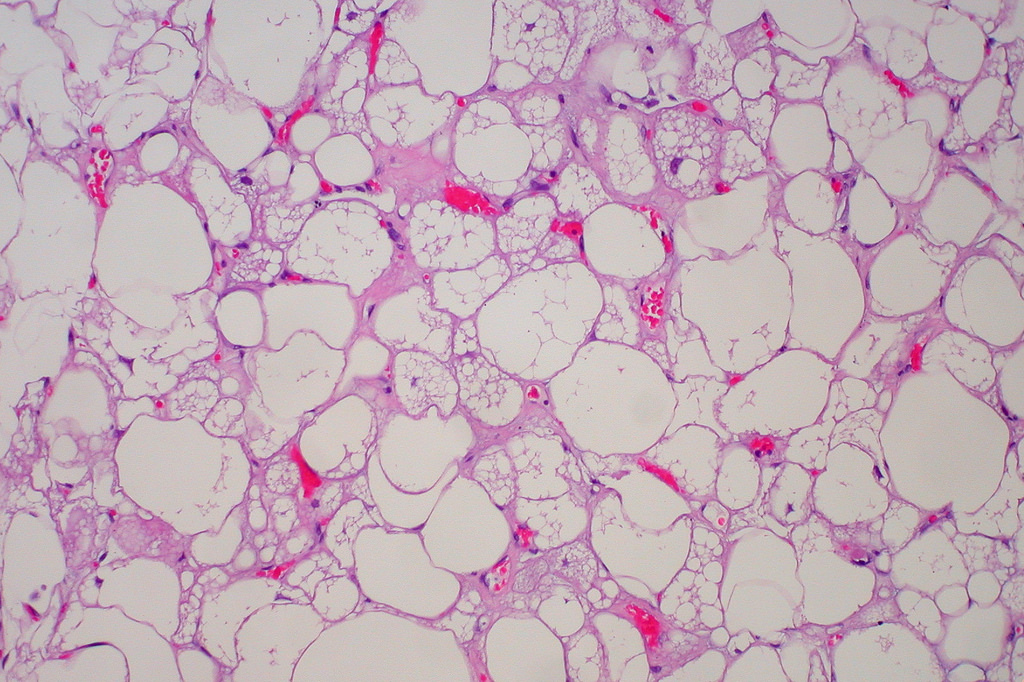
Image credit: “Hibernoma” by Ed Uthman is licensed under CC BY 2.0.